60 yr/M with LEFT LOWER LIMB WEAKNESS
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings investigations and come up with diagnosis and treatment plan
C/o-
Patient was brought to casualty with a c/o fever(high grade) since 1 week
H/o of left upper limb weakness since 7 days
H/o Dry cough since 2 days
Decreased micturation since 2 days
HOPI
Patient was apparently asymptomatic 1week back then he developed high grade fever with chills and rigors. For which he went to local RMP and was treated with some inj and medicine and fever was subsided(now subsided)
H/o dry cough since 2 days
H/o weakness of left upper limb since 1 week which is sudden in onset for which patient was admitted in miryalaguda private hospital and the patient condition was not improved and came to this institution
H/o decreased mituration from 1 week
No H/o burning micturition
No H/o of trauma
No H/o slurring of speech
Past H/o
He is a k/c/o HTN and on regular medication (tab.telma 40 mg po/oD) since 5 yrs
K/c/o DM-(TAB.METFORMIN 500MG PO/OD)since 5 yrs
No H/o Similar complaints in the past
No past surgical history
No H/o TB,asthama, thyroid, CVD,EPILEPSY
Family history-not signification
Personal history-
Farmer by occupation
Normal appatite
Mixed diet
Regular Bowel and Bladder movement
Sleep adequate
No H/o allergies
Addictions-he started drinking alcohol when he was 16 yrs old and used to drink occasionally and stopped 20 yrs back
General examination
Patient is conscious coherent and cooperative
No signs of pallor, icterus, cyanosis, clubbing ,lymphadenopathy and pedal edema.
Clinical images
Vitals-
Temp-98.4f
BP-120/80 mm of Hg
PR-94bpm
RR-18cpm
Spo2-98 on room air
GRBS-139
CVS-s1,s2 heard,no murmurs
Rs-BAE +,NVBS
P/A-SOFT AND NON TENDER
CNS-
Measurements- Rt Lt
U/L
L/L
TONE- U/L L/L
Rt N N
Lt hypo N
Power U/L L/L
Rt 5/5 5/5
Lt o/5 5/5
Reflex Rt Lt
B - -
T - -
S - -
K - -
A - -
P M F
Cranial nerves RT LT
1.sense of smell N N
2.visual acuity N N
Field of vision N N
Colour of vision N N
3,4,6-extraoccular movements-normal On both sides
Pupils-normal size and reacting to light on both sides
Direct and consensual light refleces normal in both sides
No nystagmus
No promises
5.sensory-sensation over the face normal On both sides
Motor-massager ,pterygoid normal
7.motor-orbicularis ocular ,orbicularis Oris,occipital frontalis,buccinator-normal on both sides
Sensory-taste over anterior 2/3rd of tongue normal On both sides
8.rinnes test-normal on both sides
Weber test-normal on both sides
9,10-uvula,palatal arch movements normal
Gag reflex-normal
Palatial reflex - normal
11.tarpezium and sternocleidomastoid-normal
12. No wasting and fasiculations of tongue
Tongue protrusion to mid line
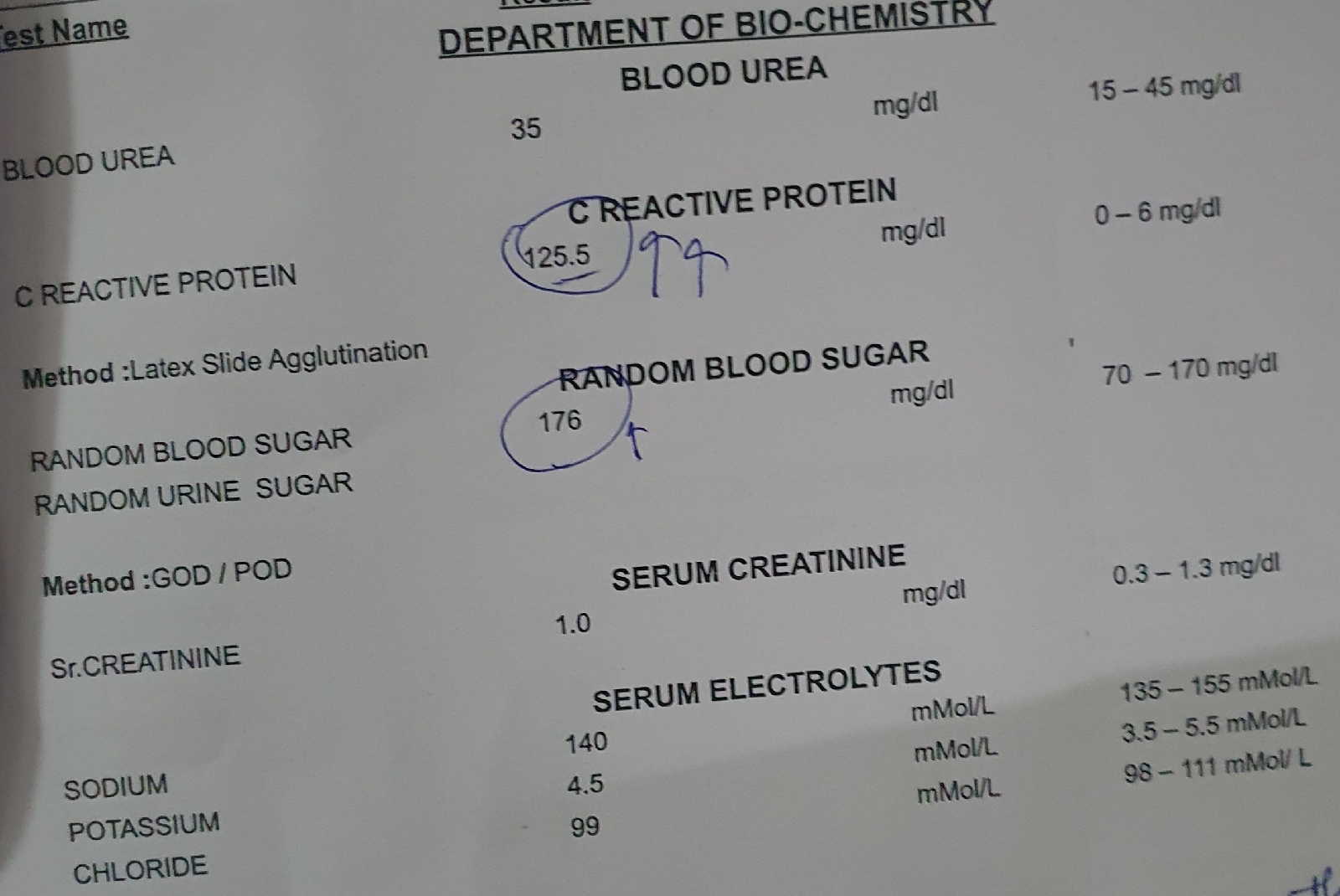
INVESTIGATIONS
left upper limb monoparesis
TREATMENT
1.inj.OPTINEURON IN 100 NS IV
2.TAB.ECOSPRIN 75 MG PO/OD
3.ATROVOSTATIN 2Omg po/oD
4. MONITORING VITALS 6TH HOURLY
5.INJ .PAN 40 MG IV
12/07/2023
Ward:General Medicine Ward
Unit:1
DOA:10/07/2023
Dr Nithhin(PGY1)
Dr Pavani(PGY2)
Dr Sushmitha (SR)
S:
Low Grade Fever ,Dry Cough
O: Patient is conscious, coherent and cooperative
No signs of pallor,icterus, cyanosis, clubbing, lymphadenopathy and pedal edema
Afebrile
Bp:140/90mm of Hg
PR:78bpm
Rr:16 cpm
Temp-100°F
Spo2-98%
CVS-S1,S2 + ;no murmurs
RS-BAE +,NVBS
P/A-SOFT AND NON TENDER
CNS-
B/L pupils NSRL
TONE- U/L L/L
Rt N N
Lt hypo N
Power U/L L/L
Rt 5/5 5/5
Lt o/5 5/5
Reflex Rt Lt
B - -
T - -
S - -
K - -
A - -
P M F
A:
Left Upper Limb Monoplegia 2°to Chronic Infarct In CapsuloGanglionic Region .
K/C/O HTN, DM type 2 since 5 years
P:
1.inj.OPTINEURON IN 100ml NS IV/OD
2.Inj.NEOMOL 100ml/IV /SOS
3.Tab.PCM 650mg PO/ BD
4.Tab.PAN 40mg PO OD
5.Tab.ECOSPRIN 75mgPO/HS
6.Tab.ATORVAS 20mg PO/HS
7.Syp.ASCORYL-LS 5ml PO/TID
8.Tab.METFORMIN 500mg PO/OD
9.Tab.TELMA 40mg PO/OD
10.Monitor Vitals 4th hrly
11.Inform SOS























Comments
Post a Comment